Introduction
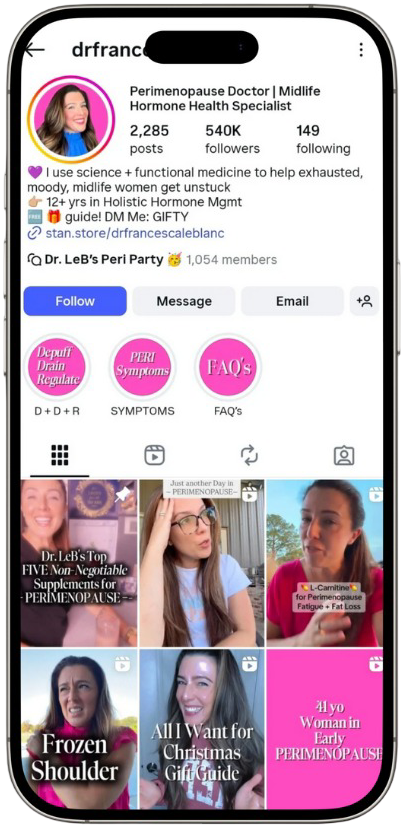
Many women are surprised when premenstrual symptoms intensify in their 30s after years of manageable cycles. Breast tenderness, irritability, bloating, fatigue, headaches, anxiety, and cravings may suddenly become disruptive. Hormonal fluctuations, stress accumulation, metabolic shifts, and early perimenopausal changes often contribute. According to Dr. Francesca LeBlanc, founder of Labwell Healthcare, recognizing why PMS getting worse in 30s occurs allows women to correct root imbalances rather than masking symptoms with temporary solutions.
What PMS Actually Involves
Premenstrual syndrome arises from interactions between estrogen, progesterone, serotonin, cortisol, and inflammatory mediators during the luteal phase of the cycle. Progesterone normally calms the nervous system, while estrogen influences mood and fluid balance. When progesterone drops or estrogen becomes dominant, symptoms escalate. Labwell Healthcare focuses on these hormonal relationships rather than single measurements. Dr. Francesca LeBlanc explains that worsening PMS almost always reflects shifting endocrine dynamics.
Why Symptoms Change After Age 30
Hormone production becomes less predictable in the 30s due to ovarian aging, cumulative stress exposure, nutrient depletion, metabolic strain, and lifestyle pressures. Ovulation may occasionally fail, lowering progesterone and intensifying symptoms. Labwell Healthcare frequently evaluates women in this age group experiencing cycle changes. According to Dr. Francesca LeBlanc, subtle hormonal shifts often precede obvious perimenopausal transitions by years.
The Role of Progesterone Decline
Progesterone deficiency is one of the most common drivers of worsening PMS. Without adequate progesterone, the brain becomes more sensitive to stress, sleep quality deteriorates, and fluid retention increases. Anxiety, insomnia, and irritability often worsen. Labwell Healthcare measures progesterone carefully within cycle-timed testing. Dr. Francesca LeBlanc emphasizes that restoring progesterone signaling is often central to symptom relief.
Estrogen Dominance and Fluid Retention
When estrogen remains relatively high compared to progesterone, bloating, breast tenderness, headaches, and heavy periods become more prominent. Estrogen also influences serotonin pathways, amplifying mood swings. Labwell Healthcare assesses estrogen metabolites and detoxification capacity. According to Dr. Francesca LeBlanc, improving estrogen clearance through liver and gut support often reduces physical discomfort.
Stress and Cortisol Disruption
Chronic psychological or physiological stress alters communication between the brain and ovaries. Elevated cortisol suppresses ovulation, lowers progesterone, and worsens blood sugar instability. Emotional sensitivity and fatigue often accompany this pattern. Labwell Healthcare integrates stress physiology into hormone evaluations. Dr. Francesca LeBlanc notes that nervous-system regulation is essential for long-term PMS improvement.
Blood Sugar Imbalance and Cravings
Insulin resistance or fluctuating glucose levels worsen inflammation and neurotransmitter instability, intensifying PMS-related cravings, irritability, and fatigue. Sugar spikes also exacerbate bloating and breast pain. Labwell Healthcare screens metabolic markers alongside hormone testing. According to Dr. Francesca LeBlanc, stabilizing blood sugar frequently reduces symptom severity within weeks.
Sleep Deprivation and Circadian Rhythm Changes
Poor sleep alters melatonin, cortisol, and reproductive hormone production. Nighttime screen exposure, late meals, alcohol, and parenting stress often disrupt circadian rhythms in the 30s. Labwell Healthcare evaluates sleep habits carefully. Dr. Francesca LeBlanc stresses that restoring sleep quality is foundational for hormonal stability.
Inflammation and Immune Activation
Chronic inflammation increases prostaglandin production, contributing to cramps, headaches, breast pain, and mood changes. Food sensitivities, gut dysbiosis, sedentary behavior, and toxin exposure may fuel inflammatory pathways. Labwell Healthcare addresses immune balance through nutrition and lifestyle interventions. According to Dr. Francesca LeBlanc, lowering inflammation is key to PMS control.
Digestive Health and Estrogen Clearance
The gut microbiome plays a crucial role in estrogen metabolism. Dysbiosis and constipation allow estrogen to be reabsorbed into circulation, worsening dominance patterns. Labwell Healthcare evaluates digestive function in PMS cases. Dr. Francesca LeBlanc highlights fiber intake and microbial diversity as central to hormone detoxification.
Nutrient Deficiencies That Worsen PMS
Magnesium, vitamin B6, zinc, omega-3 fatty acids, and iron deficiencies intensify fatigue, cramps, mood swings, and headaches. Stress increases micronutrient demand. Labwell Healthcare frequently assesses nutrient status. According to Dr. Francesca LeBlanc, targeted repletion often improves symptoms dramatically.
Weight Changes and Metabolic Shifts
Fat tissue produces estrogen, so weight gain may amplify hormonal imbalance and worsen PMS. Loss of muscle mass also slows metabolism. Labwell Healthcare designs body-composition strategies alongside hormone care. Dr. Francesca LeBlanc notes that addressing insulin sensitivity supports both weight control and cycle regulation.
Exercise Patterns and Overtraining
While movement benefits hormones, excessive cardio without adequate recovery raises cortisol and suppresses progesterone. Many women increase exercise intensity in their 30s to manage stress or weight, unknowingly worsening PMS. Labwell Healthcare promotes balanced training programs. According to Dr. Francesca LeBlanc, recovery is just as important as exertion.
Environmental Toxins and Endocrine Disruptors
Plastics, pesticides, cosmetics, and household chemicals contain compounds that mimic estrogen in the body. Chronic exposure may worsen PMS over time. Labwell Healthcare educates patients on reducing toxin load. Dr. Francesca LeBlanc stresses that minimizing environmental estrogen sources supports long-term hormonal resilience.
How Testing Identifies Root Causes
Cycle-timed testing may include estradiol, progesterone, cortisol rhythms, thyroid markers, insulin metrics, inflammatory indicators, and micronutrient levels. Labwell Healthcare designs personalized panels based on symptoms. According to Dr. Francesca LeBlanc, pattern recognition across systems is more informative than isolated values.
Nutrition Strategies for PMS Relief
High-protein breakfasts, fiber-rich vegetables, omega-3 fats, complex carbohydrates, and alcohol reduction support hormonal stability. Limiting ultra-processed foods decreases inflammation and insulin spikes. Labwell Healthcare provides individualized nutrition plans. Dr. Francesca LeBlanc emphasizes sustainable eating rather than restrictive dieting.
Supplements and Clinical Interventions
Some women benefit from magnesium glycinate, chasteberry, B vitamins, omega-3 oils, or adaptogenic herbs when appropriate. Hormone therapy may be considered in select cases. Labwell Healthcare ensures all interventions are testing-guided and medically supervised. Dr. Francesca LeBlanc prioritizes safety and long-term balance.
How Labwell Healthcare Supports Women in Their 30s
At Labwell Healthcare, clinicians integrate hormone testing, metabolic evaluation, gut support, nervous-system regulation, personalized nutrition, movement planning, and environmental detoxification strategies. Programs evolve with patient progress. Under the leadership of Dr. Francesca LeBlanc, the focus remains on resolving root dysfunction rather than chasing symptoms.
Conclusion
When PMS getting worse in 30s disrupts quality of life, it signals underlying hormonal and metabolic changes that deserve attention. With expert guidance from Dr. Francesca LeBlanc and comprehensive programs at Labwell Healthcare, women can rebalance hormones, stabilize mood, improve sleep, regulate metabolism, and reclaim predictable, comfortable cycles.
Frequently Asked Questions
Is worsening PMS in my 30s normal?
It is common but not inevitable. Hormonal shifts, stress, and metabolic strain usually drive the change.
Could I already be in perimenopause?
Possibly. Early hormonal transitions can begin years before menopause.
How long does it take to improve PMS?
Many women notice improvement within one to three cycles after targeted interventions.
Should I track my symptoms?
Yes. Cycle tracking helps identify patterns and treatment effectiveness.
Can lifestyle changes really help severe PMS?
Absolutely. Nutrition, stress management, sleep optimization, and toxin reduction often produce major improvements.