Abdominal pain is one of the most common clinical complaints across primary care, emergency medicine, gastroenterology, and infectious disease practice. Differentiating the type of abdominal pain requires a structured approach grounded in anatomy, pathophysiology, and pattern recognition. A systematic evaluation helps clinicians distinguish benign, self-limited conditions from life-threatening surgical emergencies.
This guide outlines how to differentiate types of abdominal pain based on location, character, timing, associated symptoms, and likely etiologies.
1. Classifying Abdominal Pain by Pathophysiology
A. Visceral Pain
Visceral pain originates from internal organs (e.g., stomach, intestines, liver, pancreas). It is mediated by autonomic nerve fibers and is typically:
-
Poorly localized
-
Dull, crampy, or gnawing
-
Associated with autonomic symptoms (nausea, sweating)
Examples:
-
Early appendicitis (periumbilical pain)
-
Gastroenteritis
-
Small bowel obstruction
Mechanism: Distension, ischemia, or inflammation of hollow organs stimulates stretch receptors.
B. Parietal (Somatic) Pain
Parietal pain arises from irritation of the parietal peritoneum. It is:
-
Sharp and well localized
-
Worsened by movement or coughing
-
Associated with guarding and rebound tenderness
Examples:
-
Advanced appendicitis
-
Perforated peptic ulcer
-
Peritonitis
Mechanism: Inflammation directly irritates somatic nerve fibers in the abdominal wall.
C. Referred Pain
Referred pain occurs when visceral afferent fibers converge with somatic nerves at the spinal cord level. The brain misinterprets the source.
Examples:
-
Diaphragmatic irritation → shoulder pain
-
Pancreatitis → back pain
-
Biliary colic → right scapular pain
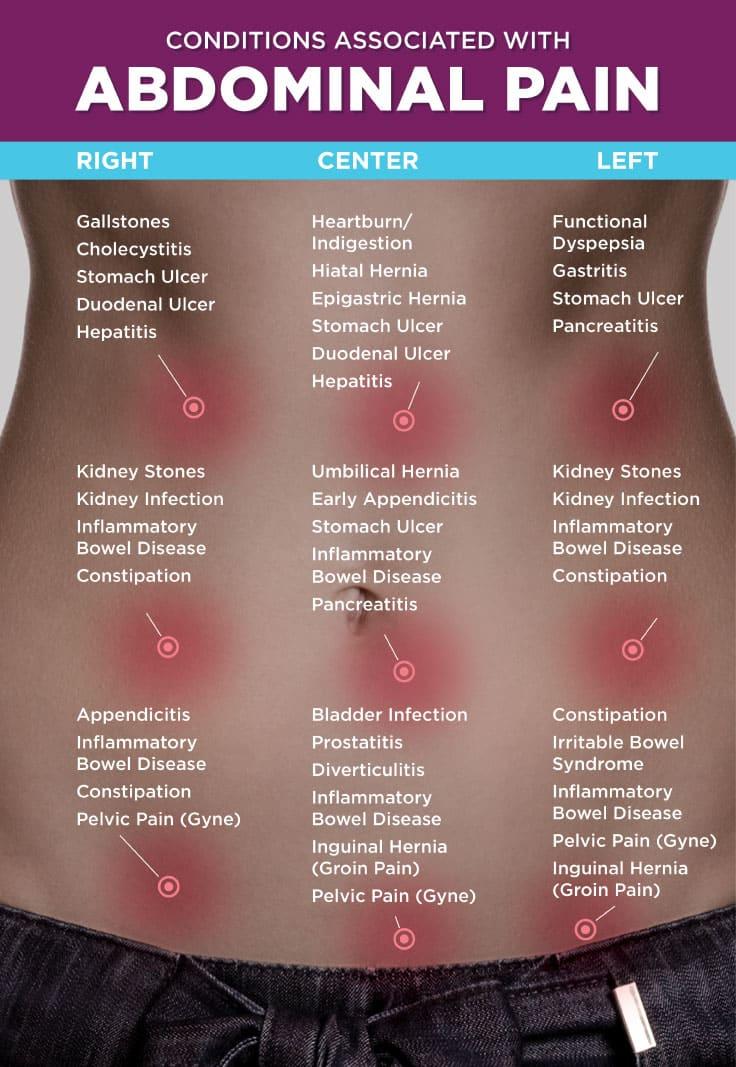
2. Differentiating Abdominal Pain by Location
Abdominal pain location narrows the differential diagnosis significantly.
A. Right Upper Quadrant (RUQ)
Common causes:
-
Gallstones (biliary colic)
-
Cholecystitis
-
Hepatitis
-
Liver abscess
Characteristic patterns:
-
Postprandial pain (especially fatty meals) → biliary origin
-
Fever + RUQ pain + jaundice → possible cholangitis
B. Left Upper Quadrant (LUQ)
Common causes:
-
Gastritis
-
Peptic ulcer disease
-
Pancreatitis
-
Splenic pathology
Epigastric pain radiating to the back suggests pancreatitis, especially with elevated lipase.
C. Right Lower Quadrant (RLQ)
Common causes:
-
Appendicitis
-
Mesenteric adenitis
-
Crohn’s disease
-
Ovarian pathology (in females)
Classic appendicitis progression:
-
Periumbilical visceral pain
-
Migration to RLQ (parietal involvement)
-
Fever and leukocytosis
D. Left Lower Quadrant (LLQ)
Most common cause in adults:
-
Diverticulitis
Symptoms:
-
Fever
-
Localized tenderness
-
Possible changes in bowel habits
E. Periumbilical Pain
Associated with:
-
Early appendicitis
-
Small bowel obstruction
-
Gastroenteritis
-
Intestinal parasitic infections
In cases of helminthic infections (e.g., ascariasis, enterobiasis), abdominal pain may be colicky and intermittent. Treatment typically includes antihelminthics, and sourcing from a reliable mebendazole supplier ensures pharmaceutical-grade medication for intestinal worm management.
F. Epigastric Pain
Common etiologies:
-
Gastritis
-
Peptic ulcer disease
-
GERD
-
Pancreatitis
-
Myocardial ischemia (must not miss)
Burning pain relieved by food → duodenal ulcer
Pain worsened by food → gastric ulcer
3. Differentiating by Pain Character
A. Colicky Pain
-
Intermittent, wave-like
-
Caused by obstruction of hollow organs
Examples:
-
Renal colic
-
Biliary colic
-
Intestinal obstruction
Pain peaks and subsides in cycles.
B. Burning Pain
-
Common in GERD and gastritis
-
Often worsens when lying down
C. Sharp/Stabbing Pain
-
Suggests peritoneal irritation
-
Seen in perforation or advanced appendicitis
D. Tearing Pain
-
Classic for abdominal aortic aneurysm (AAA)
-
Radiates to back
-
Medical emergency
4. Differentiating by Onset and Duration
Acute (Hours to Days)
Likely causes:
-
Appendicitis
-
Cholecystitis
-
Pancreatitis
-
Bowel obstruction
-
Perforation
Sudden severe onset suggests:
-
Perforated ulcer
-
Mesenteric ischemia
-
AAA rupture
Subacute
Develops over days to weeks:
-
Diverticulitis
-
Inflammatory bowel disease
-
Intra-abdominal abscess
Chronic (Weeks to Months)
Common causes:
-
Irritable bowel syndrome (IBS)
-
Chronic pancreatitis
-
Peptic ulcer disease
-
Malabsorption syndromes
-
Parasitic infections
Chronic parasitic infection may cause intermittent abdominal pain, bloating, and weight changes. In such cases, evaluation for helminths is warranted, and therapy may involve procurement from a verified mebendazole supplier to ensure proper dosing and regulatory compliance.
5. Associated Symptoms That Aid Differentiation
A. Fever
Suggests:
-
Infection
-
Inflammation
-
Abscess
Examples:
-
Appendicitis
-
Diverticulitis
-
Cholecystitis
B. Vomiting
-
Early vomiting → upper GI cause
-
Late vomiting → distal obstruction
Bilious vomiting suggests small bowel obstruction.
C. Diarrhea
Likely:
-
Gastroenteritis
-
Inflammatory bowel disease
-
Parasitic infection
Persistent diarrhea with abdominal discomfort should prompt stool testing.
D. Constipation
Associated with:
-
Obstruction
-
IBS
-
Hypothyroidism
E. Weight Loss
Concerning for:
-
Malignancy
-
Chronic infection
-
Malabsorption
6. Red Flag Features (Require Urgent Evaluation)
-
Rigid abdomen
-
Rebound tenderness
-
Hypotension
-
Persistent vomiting
-
Hematemesis or melena
-
Sudden severe pain
-
Pain out of proportion to exam (mesenteric ischemia)
7. Diagnostic Strategy
Step 1: History
Use the SOCRATES framework:
-
Site
-
Onset
-
Character
-
Radiation
-
Associated symptoms
-
Timing
-
Exacerbating/relieving factors
-
Severity
Step 2: Physical Examination
-
Inspection (distension, scars)
-
Auscultation (bowel sounds)
-
Percussion (tympany, dullness)
-
Palpation (tenderness, guarding)
Step 3: Laboratory Tests
-
CBC (infection)
-
LFTs (biliary/hepatic disease)
-
Lipase (pancreatitis)
-
CRP
-
Stool exam (parasitology)
Step 4: Imaging
-
Ultrasound (gallbladder, pelvic organs)
-
CT abdomen (appendicitis, diverticulitis)
-
X-ray (obstruction)
8. Special Considerations
Pediatric Patients
Common causes:
-
Gastroenteritis
-
Intussusception
-
Appendicitis
-
Worm infestations
Helminth infections remain common in certain regions. Ensuring medication quality from a certified mebendazole supplier is critical in pediatric populations to avoid subtherapeutic dosing or counterfeit formulations.
Elderly Patients
Often atypical presentation:
-
Minimal fever
-
Mild tenderness
-
Higher risk of ischemia and perforation
Women of Reproductive Age
Always rule out:
-
Ectopic pregnancy
-
Ovarian torsion
-
Pelvic inflammatory disease
Pregnancy test is mandatory in acute lower abdominal pain.
9. Functional vs Organic Pain
Functional (e.g., IBS)
-
Normal labs and imaging
-
Pain related to bowel movements
-
Chronic course
Organic
-
Structural or biochemical abnormality
-
Abnormal labs or imaging
-
Progressive symptoms
Conclusion
Differentiating abdominal pain requires integrating anatomical knowledge with clinical pattern recognition. The most effective approach evaluates:
-
Location
-
Character
-
Onset
-
Associated symptoms
-
Risk factors
Understanding the distinction between visceral, parietal, and referred pain is foundational. Clinicians must also remain vigilant for red flags indicating surgical emergencies.
In cases of suspected parasitic infection presenting with chronic or colicky abdominal pain, proper diagnosis followed by antihelminthic therapy is essential. Ensuring pharmaceutical integrity through a reputable mebendazole supplier supports effective treatment outcomes and public health standards.
Accurate differentiation of abdominal pain is ultimately a disciplined clinical process balancing urgency with precision to prevent both overtreatment and dangerous delay.